This advice is supported by NHS England. If you have had a Splenectomy and there are no other issues then please follow this guidance.
Practical guidance for the management of adults with Immune Thrombocytopenia during the COVID-19 pandemic
Pavord S, Cooper N, Thachil J, Hunt B, Murphy M, Lowe G, Laffan M, Makris M, Newland A, Provan D, Grainger J, Hill Q.
16th April 2020
This document aims to provide practical guidance for the assessment and management of patients with thrombocytopenia, with a particular focus on Immune Thrombocytopenia (ITP) during the COVID-19 pandemic. The intention is to support clinicians and, although recommendations have been provided, it is not a formal guideline. Nor is there sufficient evidence base to conclude that alternative approaches to treatment are incorrect. Instead, it is a consensus written by clinicians with an interest in ITP or coagulation disorders and reviewed by members of the UK ITP forum. It is a live document and will be updated as new information arises.
Background
The current COVID-19 pandemic, caused by a novel coronavirus (SARS-CoV-2), poses a number of dilemmas for the investigation of thrombocytopenia and the management of patients with ITP.
This includes consideration of the advantages and disadvantages of the standard therapeutic options for new or relapsed acute ITP, and the recognition of the challenge posed to the management of ITP patients because of both bleeding and thrombotic risks seen in patients hospitalised with COVID-19 infection. Furthermore, patients are often unclear about the extent of required self-isolation procedures.
Thrombocytopenia and COVID-19
Thrombocytopenia was described in 36% of patients hospitalised with COVID-19 in one of the early papers (Guan et al., 2020), although subsequent studies have not confirmed this high frequency. The hyper-inflammatory state and cytokine storm induced by the viral infection results in a prothrombotic state and likely endothelial and platelet activation occurs. The use of antibiotics, antivirals, heparin and other commonly used agents contributes to thrombocytopenia, as well as haemodialysis and extracorporeal membrane oxygenation (ECMO). Platelet production may be affected by direct viral insult to the bone marrow and potentially impaired fragmentation of megakaryocytes due to COVID-19 induced damage to the lung and pulmonary capillary bed (as this may be a site of platelet production). In end stage COVID-19 infection multi organ failure may exacerbate thrombocytopenia and pooled results of nine studies revealed that the platelet count was lower in patients with very severe COVID-19 (p<0.001) and that thrombocytopenia was associated with a three-fold enhanced risk of worsening disease (Lippi et al 2020). This is perhaps not unexpected as other studies of critically ill patents show thrombocytopenia to be a marker of poor clinical outcome (Nijsten et al., 2000). Huang et al found 20% of COVID-19 patients who died had a platelet count <100 x 10 9/l, compared with 1% of survivors (p<0.0001) (Huang et al., 2020).
Despite the numerous potential causes of thrombocytopenia in COVID-19 positive patients, a count below 100 x 10 9/l is unusual, only occurring in around 5% of hospitalised patients and 8% of those on ITU (Huang et al., 2020). Postulated mechanisms for the relative preservation of platelet count is increased thrombopoietin production from liver stimulation and megakaryocytes in the lung producing large amounts of platelets. Very low platelet counts of <20 x 10 9/l, or a sudden fall in the platelet count >50% over 24-48 hours is likely to indicate an immune aetiology, although this can also occur in the pre-terminal stages of COVID-19. Other causes such as thrombotic thrombocytopenia purpura and atypical haemolytic uraemia syndrome should be considered if there is associated microangiopathic haemolytic anaemia (MAHA) and, in the former, an ADAMTS13 level <10%. Experience of testing in COVID-19 without TTP, has found ADAMTS13 levels of 20-40%, typical of other inflammatory states. Drug induced thrombocytopenia develops at a median of 14 days after the onset of a new drug or sooner if there has been previous exposure. Heparin induced thrombocytopenia (HIT) occurs between 5 and 10 days after the first exposure, or within 24 hours of recurrent exposure. Autoimmune thrombocytopenia is a diagnosis of exclusion, there being no confirmative test.
Recommendation
Thrombocytopenia in COVID-19 positive patients is likely to be multifactorial.
Very low platelet counts of <20 x 10 9/l, or a sudden fall in the platelet count >50% over 24-48 hours may indicate an immune aetiology.
Other causes of immune thrombocytopenia, such as HIT, MAHA and drugs, should be considered before a diagnosis of ITP is made.
Thrombotic risk associated with ITP
ITP is associated with a mild elevation in thrombotic risk, with a cumulative incidence of 3.2% for arterial
(95% CI, 2.0–5.0) and 1.4% (95% CI, 0.8–2.5) for venous thrombosis at 5 years (Ruggeri et al., 2014). It is unknown how this combines with the many other risk factors for thrombosis in patients hospitalised with COVID-19 and whether the increment is negligible or synergistic. Risk of thrombosis in ITP patients may be slightly heightened by treatment-related factors such as splenectomy and TPO RAs and is higher where there are associated antiphospholipid antibodies.
Recommendation
One should be mindful of a potential further increased thrombotic risk in patients with COVID-19 from ITP or its treatment, although currently this is unknown.
Management of new/relapsed ITP
Like all viral infections, COVID-19 may trigger a new presentation of ITP, as illustrated in a recently published case report (Zulfiqar, 2020), or it may cause relapse in an existing patient. The need to actively treat ITP is unchanged from current consensus guidelines (Provan D et al., 2019) however, the additional potential burden of treatment in the context of the COVID-19 pandemic (for example greater hospital contact and immunosuppression and/or thrombotic risk) need to be carefully balanced against the risks of bleeding from ITP. Treatment decisions may differ depending whether the patient is COVID-19 negative or positive.
First line therapy
Standard first line therapy for the management of new or relapsed acute ITP is prednisolone, given at a dose of 1mg/kg (max 80mg) for 2 weeks and thereafter tapered off, slowly if there is a good response, or rapidly if treatment is ineffective (Provan D et al., 2019).
There are few data to inform whether or not steroids pose a higher risk of the development of COVID-19 infection or worsening symptoms once infected. However, current guidance from the WHO is to avoid steroids if there are alternative treatment options (WHO 2020). In patients who are negative for COVID-19 infection, using thrombopoietin receptor agonists (TPO-RAs) as first line therapy may be the preferred option. This use is off-label and local funding may need to be sought through the COVID-19 Interim Measures scheme. One should be mindful that TPO-RAs can take 10-14 days before an effect is seen and if urgent platelet elevation is needed, intravenous immunoglobulin may be required.
For patients who are COVID-19 positive, the treatment dilemma is even more pronounced. A concern with the use of TPO-RAs for initial treatment is the increased thrombotic potential, which might exacerbate venous thromboembolic risk in a patient with COVID-19. Steroids may be the preferred option for initial treatment. There is concern about higher risks of mortality and secondary infection which were shown in a systematic review of observational studies of corticosteroids in patients with influenza; however, most related to high steroid doses (>40mg methylprednisolone per day) and the evidence was judged as very low to low quality, owing to confounding by indication (Lansbury et al., 2019). Another study that addressed this limitation by adjusting for time-varying confounders found no effect on mortality (Delaney et al., 2016). Finally, a recent study of patients receiving corticosteroids for MERS used a similar statistical approach and found no effect of corticosteroids on mortality but delayed clearance of MERS-CoV from the lower respiratory tract (Arabi et al., 2018).
Whilst further evidence is awaited, steroids may be the better option for COVID-19 positive patients presenting with new or relapsed ITP, however the dose and duration of treatment should be kept to the minimum necessary. Starting doses of 20mg daily (whatever the patient’s weight) may be considered in non-bleeding patients, and increasing after 3-5 days if no response. Long courses of steroids should be avoided, and the usual recommendation of tapering after 2 weeks should be adhered to.
Thrombopoietin receptor agonists
Current licensed TPO-RAs used in the UK include romiplostim and eltrombopag. They are effective in stimulating platelet production, with responses seen from 7 -10 days in the majority of cases.
Concern has been raised regarding their prothrombotic potential. This was supported by a recent in vitro study of samples from 26 patients which showed that those with ITP had increased microvesicle-associated thrombin generation two weeks after initiation of TPO-RA-treatment compared with controls and pre-treatment levels (Garabet et al., 2020).
Systematic review of trials looking at clinical thromboembolic events has found higher rates in patients on TPO RAs compared with controls (Catala-Lopez et al., 2012) and a long-term clinical study of eltrombopag showed 6% of patients developed arterial or venous thrombosis (Wong et al., 2017). There are similar findings with romiplostim but direct comparison with placebo, showed no increase in thrombotic risk (Cines et al., 2017, Kuter et al., 2019), however, as expected, risk of thrombosis increases with age (Kuter et al., 2019).
Hepatobiliary events have been found to occur in 15% of patients on eltrombopag (Wong et al., 2017) and the drug carries a black box warning for risk for hepatotoxicity. Although clinically significant liver injury has reported to be uncommon in COVID-19 (Bangash et al., 2020), liver enzymes are usually elevated and the required monitoring of liver function tests throughout treatment with eltrombopag (Promacta®, 2018, Revolade, 2018), would be complicated. Although there are no data on the use of TPO-RAs in COVID-19 positive patients, the risk of hepatotoxicity and potential for increased thrombosis would prompt caution with their use in this setting.
Intravenous Immunoglobulin
Intravenous immunoglobulin (IvIg) may be necessary if immediate elevation of the platelet count is required to control bleeding, although this cannot be relied upon as indicated in a recent case report of ITP occurring in the context of COVID-19 infection (Zulfiqar, 2020). IvIg may also be used as second line treatment if there is failure to respond to steroids. Response usually lasts for 6 weeks or more and may be long enough to cover the worst of the pandemic period. However, administration requires hospital attendance, supply is short and whilst clinical complications are rare, they can be significant.
The role IvIg may play in the management of patients with severe COVID-19 infection is unknown. A small retrospective study from Wuhan suggested that initiation of IVIG as adjuvant treatment for COVID-19 pneumonia within 48 hours of admission to intensive care may reduce the use of mechanical ventilation and promote earlier recovery of patients (Xie et al., 2020). Larger studies are required before any recommendations can be made of the use of IvIg for COVID-19 infection.
Tranexamic acid
Tranexamic acid (TXA) inhibits fibrinolysis and while it is contraindicated in frank DIC, the COVID-19 associated coagulopathy (CAC) does not fulfil the ISTH criteria for DIC. However localised fibrin thrombi occur in the alveolar capillaries and small vessels in association with inflammation and alveolar damage (Fox et al., 2020), and endogenous fibrinolysis breaking down the disseminated thrombi could theoretically aid recovery from this. Therefore, in a bleeding patient with COVID-19 disease, judgement should be made regarding the balance of risks associated with bleeding and thrombosis. If tranexamic acid is used, the duration of treatment should be kept to the minimum necessary. For oral bleeding, tranexamic acid mouthwashes can be given to rinse and spit out.
Interestingly, a recent report in Physiological Reviews proposed that the endogenous protease plasmin acts on COVID-19 virus by cleaving a newly inserted furin site in the S protein portion of the virus resulting in increased infectivity and virulence (Ji et al., 2020). Blunting of this response with tranexamic acid has been postulated to reduce infectivity of the virus and an exploratory, randomised, placebo-controlled, double-blind Phase 2 clinical trial is being established (Ness, 2020).
Immunosuppressant drugs and rituximab
There is concern that immunosuppressant drugs and rituximab increase risk of COVID-19 infection and these should be avoided in new or relapsed patients during the COVID-19 pandemic if possible.
Platelet transfusions
Platelet transfusions are not usually necessary or helpful and should not be routinely offered to thrombocytopenic COVID-19 patients who are not bleeding. In patients with immune thrombocytopenia they are likely to be consumed too quickly to be of value. Platelet transfusions should only be given if it is considered that haemorrhage is life-threatening or in a critical site such as the eyes
Recommendation
There is little evidence to inform the optimal management of a patient presenting with new or relapsed acute ITP.
In patients who are negative for COVID-19, TPO-RAs may be preferred as first line treatment, to avoid corticosteroids which may increase risk of COVID-19 infection during the pandemic.
In patients who are positive for COVID-19, TPO-RAs may potentially increase the thrombotic complications or hepatotoxicity and should be avoided if possible. For these patients steroids may be the preferred option.
If steroids are used as first line therapy, the dose and duration should be kept to the minimum necessary.
Starting dose of 20mg daily may be considered in non-bleeding patients, with increase to 1mg/kg after 3-5 days if there has been no response.
Steroid doses should be tapered after 2 weeks – slowly if there has been good response, rapidly if there is no response.
Intravenous immunoglobulin (1g/kg) may be necessary if immediate elevation of the platelet count is required to control bleeding. It may also be used as second line treatment if there is failure to respond to steroids.
Tranexamic acid in COVID-19 infected patients should be used as required for the management of bleeding in ITP patients, but avoided in those with frank DIC.
Platelet transfusions should only be given if bleeding is thought to be life threatening, or at a critical site.
Management of chronic ITP
Management of patients with chronic stable ITP should not alter because of the pandemic, patients should remain on their current medication, even if this includes steroids and immunosuppressants. However attention to isolation procedures is crucial. The British Society for Rheumatology provides helpful guidance on shielding measures for patients on immunosuppressants (Figure 1).
Patients with splenectomy are probably not at increased risk of COVID-19 infection but are susceptible to bacterial infections and must be vigilant with their prophylactic antibiotics during this time and up to date with their pneumococcal, haemophilus influenza and meningitis vaccinations.
ITP patients not requiring treatment in the last 12 months, or on non-immunosuppressive agents such as thrombopoietin receptor agonists, are not considered to be at increased risk of COVID-19 infection and should comply with self-isolation measures as for all individuals in the UK.
Recommendation
Patients with chronic ITP should remain on their usual treatment.
They should be vigilant with self-isolation and shielding measures as appropriate.
Splenectomised patients should be stringent with their antibiotic prophylaxis and up to date with vaccinations.
Regular patient contact should be maintained and appointments conducted by telephone or online platforms.
Thromboprophylaxis in hospitalised COVID-19 patients
Potential risk factors for venous thrombosis in patients hospitalised with COVID-19 include infection, immobilisation, respiratory failure, mechanical ventilation, and central venous catheter use. Those with or without ITP should be considered for venous thromboprophylaxis, according to NICE guidance. This needs to be balanced against the bleeding risk which is seen in some patients with severe COVID-19 infection, even without thrombocytopenia (Wang T et al., 2020). Low molecular weight heparin is the preferred anticoagulant, with clinical trials showing it to be more efficacious than UFH. It also has anti-complement and anti-inflammatory properties. LMWH should be avoided if platelets are <30 x 10 9/l and intermittent pneumatic compression should be used. The LMWH should be recommenced once the platelet count can be raised above this threshold. Regular assessment of both bleeding and thrombotic risk is essential throughout the course of the hospital stay and upon discharge.
Recommendation
ITP patients hospitalised with COVID-19 should receive LMWH thromboprophylaxis provided platelets are >=30 x 10 9/l and there are no haemorrhagic features.
ITP patients hospitalised with COVID-19 whose platelets are <30 x 10 9/l should receive intermittent pneumatic compression alone until their platelet count recovers.
Patient information
This is an anxious time for everyone and not least for those with autoimmune diseases. Contact with patients is important and reassurance that services will continue as normal but that outpatient appointments will be conducted by telephone or online F2F platforms wherever possible. Arrangements for blood tests and safe pick-up or delivery of medications should be made clear.
They should be provided with information regarding self-isolation procedures and shielding (Figure 1), maintaining mental well-being, and who to contact if they are feeling unwell with fever and cough or are having difficulty breathing.
They should also be made aware that COVID-19 infection, like all viral infections, may cause a relapse of their ITP and informed who to contact if they think their platelet count has dropped or if they experience bleeding or unusual bruising.
Recommendation
Hospital attendance should be kept to the minimum necessary, with outpatient appointments conducted by telephone or online face to face platforms where possible.
Patients should be provided with information regarding self-isolation and shielding procedures and given contact arrangements for COVID-19 related symptoms or suspected ITP relapse.
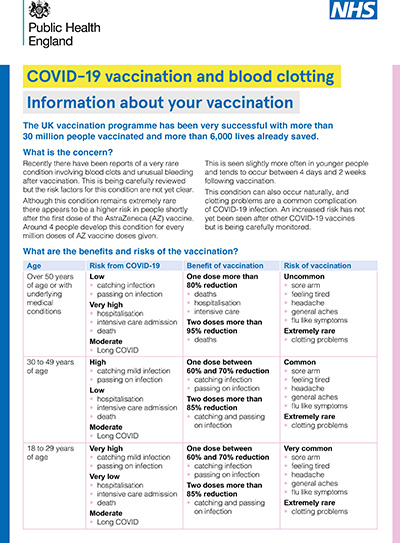
Figure 1
|
Patients who should be shielding
The Government strongly advises people with serious underlying health conditions to follow shielding measures. Guidance from the British Society for Rheumatology suggests inclusion of the following immunosuppressant regimes
• Corticosteroids ≥20mg (0,5mg/kg) prednisolone, or equivalent, per day for > 4 weeks
• Corticosteroid dose of ≥5mg prednisolone (or equivalent) per day for >4 weeks plus at least one other immunosuppressive medication (e.g. azathioprine, mycophenolate, ciclosporin) or rituximab within the last 12 months.
• A combination of 2 immunosuppressive medications including rituximab within the last 12 months plus an additional co-morbidity (age >70, Diabetes Mellitus, any pre-existing lung disease, renal impairment, any history of Ischaemic Heart Disease or hypertension).
• Splenectomy and ongoing immunosuppressive agents. (Authors’ added guidance)
Shielding measures include
1. Staying in the home and receiving deliveries of food and medicines as necessary.
2. Strict avoidance of contact with someone who is displaying symptoms of COVID-19.
3. Avoiding gatherings, including friends and families in private places
4. Using remote technology for contact (phone, internet, social media).
5. Register for the Government helpline for vulnerable people www.gov.uk/coronavirusextremely-vulnerable or call 0800 0288327
|
References
Arabi, Y.M., Mandourah, Y., Al-Hameed, F., et al. (2018) Corticosteroid therapy for critically ill patients with Middle East respiratory syndrome. American Journal of Respiratory and Critical Care Medicine, 197:757-767. doi: 10.1164/rccm.201706-1172OC. PMID: 29161116.
Bangash, M., Patel, J., Parekh, D. (2020) COVID-19 and the liver: little cause for concern. The Lancet Gastroenterology and Hepatology, 20 March. DOI:https://doi.org/10.1016/S2468-1253(20)30084-4.
Catala-Lopez, F., Corrales, I., Martin-Serrano, G., Tobias, A., Calvo, G. (2012) Risk of thromboembolism with thrombopoietin receptor agonists in adult patients with thrombocytopenia: systematic review and meta-analysis of randomized controlled trials. Medicina Clinica, 139: 421-429.
Cines, D.B., Wasser, J., Rodeghiero, F., et al. (2017) Safety and efficacy of romiplostim in splenectomized and nonsplenectomized patients with primary immune thrombocytopenia. Haematologica, 102:1342-1351.
Delaney, J.W., Pinto, R., Long, J., et al. (2016) The influence of corticosteroid treatment on the outcome of influenza A(H1N1pdm09)-related critical illness. Critical Care. 20:75. Epub 2016/04/03. doi: 10.1186/s13054-016-1230-8. PubMed PMID: 27036638; PMCID: PMC4818504.
Fox, S.E., Akmatbekov, A., Harbert, J., Li, G., Brown, Q., Vander Heide, R.S. (2020) Pulmonary and Cardiac Pathology in COVID-19: The First Autopsy Series from New Orleans. medRxiv 2020.04.06.20050575; DOI: https://doi.org/10.1101/2020.04.06.20050575
Garabet, L., Ghanima, W., Hellum, M., et al. (2020) Increased microvesicle-associated thrombin generation in patients with immune thrombocytopenia after initiation of thrombopoietin receptor agonists. Platelets 31: 322-328, DOI: 10.1080/09537104.2019.1639655
Guan, W., Ni, Z., Hu, Y. et al. (2020) for the China Medical Treatment Expert Group for COVID-19. Clinical Characteristics of Coronavirus Disease 2019 in China. New England Journal of Medicine. February 28.
DOI: 10.1056/NEJMoa2002032
Huang, C., Wang, Y., Li, X. et al. (2020) Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China, The Lancet. 395:497–506. https://doi.org/10.1016/S0140-6736(20)30183-5.
Ji, H.L., Zhao, R., Matalon, S., Matthay, M.A. (2020) Elevated Plasmin(ogen) as a Common Risk Factor for COVID-19 Susceptibility. Physiological Reviews. 100:1065-1075. DOI: 10.1152/physrev.00013.2020. Epub 2020 Mar 27.
Kuter, D,J., Newland, A., Chong, B.H., et al. (2019) Romiplostim in adult patients with newly diagnosed or persistent immune thrombocytopenia (ITP) for up to 1 year and in those with chronic ITP for more than 1 year: a subgroup analysis of integrated data from completed romiplostim studies. British Journal of Haematology. 185:503-513.
Lansbury, L., Rodrigo, C., Leonardi-Bee, J., Nguyen-Van-Tam, J., Lim, W.S. (2019) Corticosteroids as adjunctive therapy in the treatment of influenza. Cochrane Database of Systematic Reviews, 24;2. DOI: 10.1002/14651858.CD010406.pub3.
Lippi, G., Plebani, M., Henry, B.M. (2020) Thrombocytopenia is associated with severe coronavirus disease 2019 (COVID-19)infections:A meta-analysis.ClinicaChimicaActa 506:145-148. https://doi.org/10.1016/j.cca.2020.03.022
Ness, T. (2020) Tranexamic Acid (TXA) and Corona Virus 2019 (COVID19) in Inpatients (TCInpatient). ClinicalTrials.gov: NCT04338126
Nijsten, M.W., ten Duis, H-J., Zijlstra, J. et al. (2000) Blunted rise in platelet count in critically ill patients is associated with worse outcome. Critical Care Medicine 28:3843–3846.
PROMACTA® (2018) (eltrombopag) tablets, for oral use; PROMACTA® (eltrombopag) for oral suspension [prescribing information]. East Hanover, NJ: Novartis Pharmaceuticals Corporation.
Provan, D., Arnold, D., Bussell, J. et al. (2019) Updated international consensus report on the investigation and management of primary immune thrombocytopenia. Blood Advances 3:3780–3817.
Revolade (2018). Revolade (olamine) [summary of product characteristics]. Dublin, Ireland: Novartis Europharm Limited.
Ruggeri, M., Tosetto, A., Palandri, F. et al. (2014) for the Gruppo Italiano Malattie EMatologiche dell'Adulto (GIMEMA) Anemia and Thrombocytopenias Working Party. GIMEMA Study ITP0311. Thrombotic risk in patients with primary immune thrombocytopenia is only mildly increased and explained by personal and treatment‐related risk factors. Journal of Thrombosis and Haemostasis, 12: 1266– 73.
Wang, T., Chen, R., Liu, C. et al.(2020) Attention should be paid to venous thromboembolism prophylaxis in the management of COVID-19. The Lancet Haematology. April 09. DOI:https://doi.org/10.1016/S2352-3026(20)30109-5
Wong, R., Saleh, M., Khelif, A., et al. (2017) Safety and efficacy of long-term treatment of chronic/persistent ITP with eltrombopag: final results of the EXTEND study. Blood 130: 2527–2536. DOI: https://doi.org/10.1182/blood-2017-04-748707
World Health Organisation. Clinical management of severe acute respiratory infection (SARI) when COVID-19 disease is suspected. Interim guidance 13 March 2020.
Xie, Y., Cao, S., Li, Q. (2020) Effect of regular intravenous immunoglobulin therapy on prognosis of severe pneumonia. Journal of Infection, DOI: https://doi.org/10.1016/j.jinf.2020.03.044
Zhou, F., Yu, T., Du, R. et al. (2020) Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 395:1054-1062
Zulfiqar, A-A., Lorenzo-Villalba, N. (2020) Immune thrombocytopenia in a patient with COVID-19. The New England Journal of Medicine, April 15.